
Fibula lengthening then centralization for the treatment of pseudoarthrosis at the middle third of tibia with large leg-length discrepancy – A case report
Author links open overlay panel: DoanVan Le LuongVan Nguyen
Read original article: https://doi.org/10.1016/j.ijscr.2021.106577
Highlights
• Tibial pseudoarthrosis with large leg-length discrepancy and extensive scarring was a great challenge.
• The treatment for these lesions was not defined.
• Ipsilateral fibula lengthening then centralization for the treatment of tibial pseudoarthrosis was a safe, rapid, and inexpensive procedure.
• Our procedure was not difficult, and microvascular skills and special devices were not required.
Abstract
1. Introduction and importance
Tibial dysplastic pseudoarthrosis associated with large leg-length discrepancy and extensive scarring was a great challenge for orthopedic surgeons. The treatment for these lesions was not defined.
2. Case presentation
We report a 24-year-old case of dysplastic pseudoarthrosis at the middle third of the right tibia with a 10 cm leg-length discrepancy and a 250 medial deviation and 200 internal torsion due to osteomyelitis 14 years previously. She was treated by fibula lengthening then centralization for the treatment of tibial pseudoarthrosis. Eight months after the operation, the patient reported no pain and became capable of walking without an orthosis. X-rays showed full bone union at the proximal tibiofibular synostosis and the lengthening site of the right fibula. The distal tibiofibular synostosis was healing. The range of movement of the knee and ankle was restored.
3. Clinical discussion
This technique was different from the Huntington procedure. A good union between the transposed fibula and the remaining part of the fibula brought a better strength of the reconstructed tibia. The tibial pseudoarthrosis, leg-length discrepancy, and malalignment had been solved by our techniques. The procedure was easy, rapid, and inexpensive without requiring microsurgery skills and special devices.
4. Conclusion
Leg lengthening then centralization of ipsilateral fibular graft is an excellent option for reconstruction of a tibial pseudarthrosis with a large leg-length discrepancy. It is a safe, rapid, and inexpensive procedure. The procedure was not difficult, and microvascular skills and special devices were not required.
Level of evidence
A case report.
Keywords
Tibial defect
Tibial pseudoarthrosis
Leg-lengthening
Leg-length discrepancy
1. Introduction and importance
Tibial dysplastic pseudoarthrosis with large leg-length discrepancy was a great challenge for orthopedic surgeons, especially when associated with extensive skin and soft tissue damage. The deformities of the tibia with shortened, deviation, dysplastic non-union must be solved as much as possible. The treatment for these lesions was not defined. Reconstruction of this injury could be done by various methods including segmental allograft, vascularized and non-vascularized autograft, induced membrane technique, bone transport, and Huntington procedure. Implantation of segmental allograft and non-vascularized autograft in the tibial dysplastic pseudoarthrosis with surrounding extensive scarring post-osteomyelitis may be at a high risk of failure, like infection, rejection, fractures, and nonunion. The free vascularized bone transfer had been suggested as the leading option for tibial defects of 5 to 12 cm. Although vascularized fibular autografts have distinct benefits and allow simultaneous soft tissue coverage, problems were relatively common. These included infection and stress fracture and could occur at both donor and recipient sites, the hypertrophy of the graft was unreliable. The technique also was an extensive and time-consuming procedure, which requires harvesting a contralateral fibula and microsurgery skills [1], [2]. Huntington procedure has been used for managing complex tibial nonunion with intensive tissue damage [3], [4]. It provided a large graft of the ipsilateral fibula raised on a pedicle of the peroneal artery, aligned and fixed to the tibia; avoiding exposure of the site that is vulnerable to infection and facilitated wound healing without prolonged hospitalization. The Masquelet technique was relatively ineffective in achieving union in the reconstruction of great tibial defects and was associated with a high rate of infection [5], [6]. However, the leg-length discrepancy and an acceptable limb alignment had not been solved by the abovementioned techniques [4], [7]. Leg lengthening had been done following tibial reconstruction. Bone transport also was used for massive tibial bone loss, but if the amount of bone loss was great, the time to achieve the desired length of regenerate could be extremely long with many complications. Bone transport required a one-month consolidation period for 1 cm of regenerated bone and distal consolidation between the distal and transported fragments required 6 months [8]. In patients with massive tibial bone loss, the Ilizarov technique for distraction-compression osteogenesis could be associated used with the Huntington procedure [3]. However, this method was technically demanding and had theoretical risks of complications that may occur even when performed by experienced orthopedic surgeons. Complications included pin site infection (up to 80%), loss of alignment, failure of bone consolidation, nonunion at the docking site (up to 44%) refractures, and scarring [5].
We report a 24-year-old case of tibial dysplastic pseudoarthrosis with a 10 cm leg-length discrepancy due to osteomyelitis. Our case was treated using an atypical procedure by fibular lengthening then centralization for the treatment of pseudoarthrosis at the middle third of the right tibia.
2. Case presentation
This case follows 2020 SCARE guidelines for reporting of cases in surgery [9]. A 24-year-old woman was transferred from a local hospital to our hospital with a diagnosis as pseudoarthrosis of the right tibia due to osteomyelitis. She reported a history of right tibial hematogenous osteomyelitis when she was five years old. She was treated in a local hospital and was under the intervention of removal of dead bone of the right tibia. Unfortunately, she had a purulent at the right post-operatively. She was transferred to the central hospital and had five other operations of debridement. The wound in the right leg had not been healed well until 10 years later. The right tibia had been non-union with leg length discrepancy. After that, she had not been under any treatment. As she was growing up, the shortening and deformity of her left lower leg became obvious. She could walk without crutches, but with difficulty. The patient was well. During the physical examination, upper limbs and spine were unaffected, as well as the left lower extremity. The right hip and knee were stable and normal in terms of the range of motion. There was a 250 varus and 200 internal torsion deformity of the right leg with a 10–cm-leg-length discrepancy. The anterior soft tissue at the middle third of the right leg was in poor condition with extensive scarring and the right foot was in equinovarus deformity (Fig. 1). The movement range of the right ankle was 0° dorsiflexion and 30° plantarflexion. There was no comprimisation of blood flow, sensation, or motor-nerve function. X-rays showed a dysplastic pseudoarthrosis at the middle third of the right tibia with a 10 cm leg-length discrepancy. There was a 250 medial varus and torsion deformity of the right tibia. The right fibula was hypertrophied and curved at the distal third. The ankle joint was nearly normal except for a thickened lateral malleolus. A radiograph showed the pelvis severely tilted to the right (Fig. 1). The patient had no family history of any relevant genetic information, psychosocial history, or relevant pre-existing illnesses. She did not smoke and drink alcohol.

Fig. 1. X-rays and Clinical condition pre-operative. A, B, Clinical condition pre-operative. C, D, CT Scanner of lower extremity and X rays of right tibia and fibula.
Based on her history, physical exams, and X-rays findings, it was determined that she had dysplastic pseudoarthrosis at the middle third of the right tibia with a 10 cm leg-length discrepancy and a 250 medial deviation, and 200 internal torsion due to osteomyelitis 14 years ago. After discussion of the risks and benefits of surgery, the patient decided to undergo the recommended surgical procedure: 10 cm leg lengthening using external fixater after proximal and distal fibular osteotomies and then fibular centralization for the treatment of pseudoarthrosis at the middle third of tibia. The patient underwent surgery in the supine position with spinal anesthesia. She has received a single dose of prophylactic antibiotics before thigh tourniquet inflation. The operative leg was prepared and draped in a routine surgical sterile fashion above the knee. The Nhan’s external fixater was used for leg lengthening in this case. That had been used widely in Vietnam for the management of open fracture for over 20 years.
Nhan’s external fixator was made in Vietnam. The frame consists of two vertical bars (10 mm diameter) (Fig. 1) with opposing threads (1 mm pitch) to stretch or compress the bone by turning. Each bar was 320–350 mm in length and included six operable flat faces at the center, numbered 1-2-3-4-5-6 in the direction of stretching. By rotating each vertical bar three times daily, with each turn equal to one number in the middle of the bar, the pin clamps at the proximal and distal of the bar would expand approximately 1 mm.
A 3 cm longitudinal incision was done at the lateral border of the proximal fibula. The fascia was opened then the peroneal nerve was identified and retracted laterally. The fibula neck was exposed and osteotomized using a chisel. A 2 cm longitudinal incision was done at the lateral border of the fibular distal third. The fascia was opened then the fibula was exposed and osteotomized using a chisel about 6 cm proximal to the distal fibula. The internal torsion deformity of the leg was reduced. The Nhan’s uniplanar both-side external fixater was applied at the right tibia with four Steinman pins and one Schanz pin. Two Steinman pins and a Schanz pin were inserted at the proximal third of the tibia, two Steinman pins were inserted at the distal third of the tibia. The incisions were sutured (Fig. 3). Lengthening started at day 5 with a 1/3 mm extension applied four times daily. The patient was discharged 10 days postoperatively. Before discharge, she was instructed regarding properly performing distractions at home. She was permitted partial weight-bearing activities with crutches. Seven weeks post-operatively, the distal fibula was medialized and fixed to the distal tibial segment using a lag screw. A percutaneous Achilles tendon tenotomy was done and the right foot was fixated by an external fixater at the same time to correct equinovarus deformity of the right foot. She was instructed regarding properly performing a gradual reduction of right tibial varus deformity during lengthening at home. Every three weeks follow-ups were conducted. 14 weeks post-operative, the right leg had been lengthened 10 cm. The proximal fibula was medialized and fixed to the proximal tibial segment using lag screws. The external fixater was removed and the patient applied a long-leg orthosis (Fig. 2). 18 weeks post-operative, the proximal and distal tibiofibular synostosis were applied iliac crest bone graft and the patient was permitted partial weight-bearing activities with crutches for 2 months. After that, she could walk without crutches. 8 months after the operation, the patient reported no pain and became capable of walking without an orthosis (Fig. 3). X-rays showed full bone union at the proximal tibiofibular synostosis and the lengthening site of the right fibula (Figs. 3). The distal tibiofibular synostosis was healing, it required bone graft again which she refused. The range of movement of the knee and ankle was restored. She is now checked regularly monthly by the authors. The patient reports being very satisfied with the overall results.
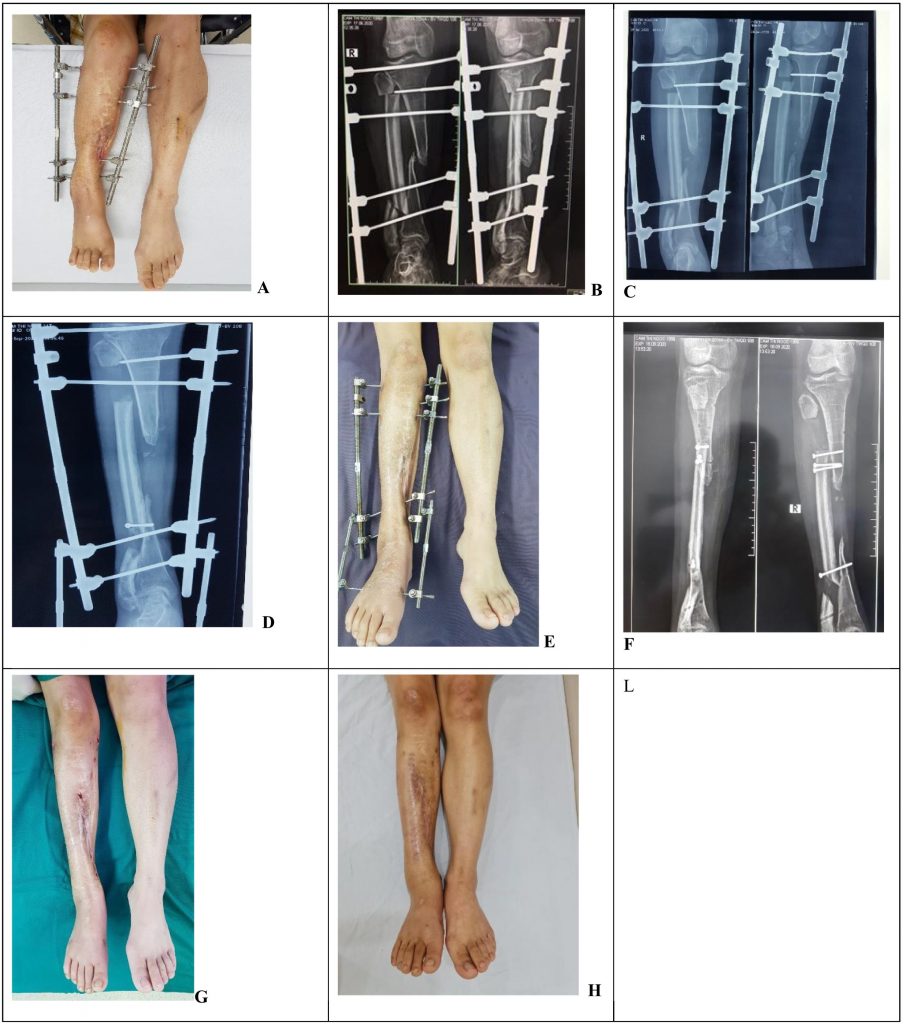
Fig. 2. X-rays and clinical condition during lengthening period. A, B, Clinical condition and X-rays post-operative. C, X-rays 3 weeks post-operative. D, E, Clinical condition and X-rays 7 weeks post-operative. F, G, Clinical condition and X-rays 14 weeks post-operative. H, Clinical condition 18 weeks post-operative.
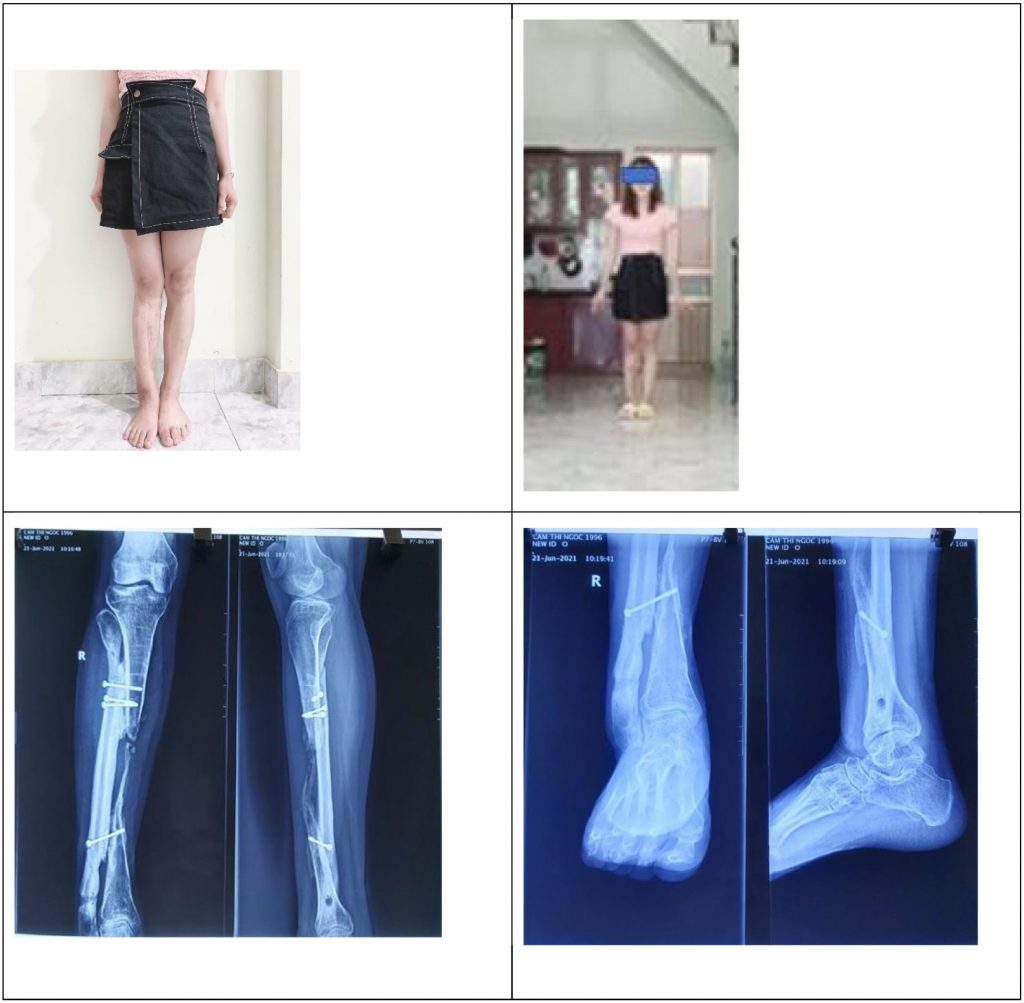
Fig. 3. Clinical condition and X-rays 8 months post-operative.
3. Discussion
Tibial pseudoarthrosis due to trauma or osteomyelitis was not rare. However, our case caused by osteomyelitis during her childhood was quite distinct from the other tibial pseudoarthrosis. It was a tibial dysplastic pseudoarthrosis at the middle third with a 250 medial deviation and 200 internal torsion of the tibia, 10 cm leg-length discrepancy, the hypertrophied curved intact fibula, and intensive scarring at the anterior tibial pseudoarthrosis. The fibula was curved and torsional at the distal third. This lesion was a great challenge for orthopedic surgeons and reconstructive surgeons. The deformities of the tibia with bone defects, dysplastic non-union, deviation, torsion, and leg length discrepancy must be solved as much as possible. It was a considerable surgical challenge, especially when associated with extensive scarring at the anterior aspect at the middle third of the leg. Management of these injuries depended on surgeon experience and training. Reconstruction of this injury could be done by various methods including large segmental allograft, vascularized and non-vascularized autograft, induced membrane technique, bone transport, and Huntington procedure.
Implantation of large amounts of allograft, induced membrane technique or non-vascularized autogenous fibular graft for reconstruction of large tibial defects had been associated with greater risk of infection, graft rejection, fracture, nonunion, and fear of disease transmission, especially when associated with extensive scarring, and the fibular graft may not undergo hypertrophy [5], [6], [10]. It also did not solve the leg-length discrepancy.
The most common methods of treating a segmental bone defect are either with the use of a vascularised fibular autograft or by bone transport using the Ilizarov technique [1]. Bone transport required a lengthy procedure which limited its use in the reconstruction of tibial defects with a big gap. If the amount of bone loss was great, the time to achieve the desired length of regenerate could be extremely long with frequent follow-ups to identify and manage various obstacles and complications such as high rate of infection, equinovarus, deviation deformity, osteomyelitis, refractures, nonunion, pain and discomfortable condition due to a long time of wearing external fixater [1], [2], [11], [12], [13].
The free vascularized bone transfer had been suggested as the leading option for tibial defects of 5 to 12 cm. However, it was an extensive and time-consuming procedure, which required harvesting a contralateral fibula and microsurgery skills. There were many other complications such as flap necrosis, deep infection, but hypertrophy of the graft was unreliable and late fracture, peroneal nerve injury [1], [2]. It also did not solve the leg-length discrepancy.
The Huntington procedure was popularized by Huntington to manage tibial defects with intensive soft tissue injury [3], [4]. It provided a large graft of the ipsilateral fibula raised on a pedicle of the peroneal artery, aligned and fixed to the tibia. The transposed fibula had muscles attached to it, along with its nutrient artery supply, this helped in the good union of the fibula that would substitute the tibia for normal activities. The Huntington procedure avoided exposure of the site that was vulnerable to infection. Both these factors helped reduce the post-operative infection. The procedure was easy to perform without requiring special equipment. However, leg-length discrepancy and malalignment were seen in all patients, and hypertrophy of the fibular graft was unreliable and late fracture [4], [7]. Catagni [3] reported two cases of tibial defects with the leg-length discrepancy in which ipsilateral fibular was gradually medial transferred using the Ilizarov apparatus combined with distal and/or proximal tibial lengthening using any residual tibial bone in the same limb. However, this method was technically demanding and had theoretical risks of complications such as neurovascular injury, infection, muscular damage, articular injury, deep venous thrombosis, refractures, deformities, and scarring.
In our cases, she had a dysplastic pseudoarthrosis at the middle third of the right tibia with a 10 cm leg-length discrepancy, a 250 medial deviation and 200 internal torsion, and extensive scarring so we combined the leg-lengthening according to Ilizarov technique and Huntington procedure for her treatment. The right leg was lengthened using an external fixater to solve leg-length discrepancy after the ipsilateral hypertrophic fibula was osteotomized at the proximal and distal third, then medialized the fibula and fixed the ipsilateral fibula to the tibia using leg screws and applied iliac bone graft. The tibial varus deformity was gradually reduced using an external fixater during lengthening. It was easy for the patient to adjust the Nhan’s external fixater at home. This frame was made in Vietnam, it was cheap and available. Our patient had been applied an iliac bone graft at the proximal and distal tibial-fibular synostosis because of the dysplastic pseudoarthrosis at the middle third of the right tibia.
We had done fibular osteotomy with the maintenance of the periosteum above and below the osteotomy. The right leg was lengthened using the external fixater. This resulted in a good union between the hypertrophy transposed fibula and the remaining part of the fibula in our case, which brought a better strength of the reconstructed tibia. This technique was different from the Huntington procedure. Our technique was an easy, rapid, inexpensive procedure without requiring microsurgery skills and a special device, with a shorter time of wearing external fixater than bone transport. The patient had to wear the frame for 14 weeks then wear the orthosis until six months post-operative. This technique had great advantages of preserving the patient’s limb, with the better psychological aspect.
Some authors encountered iatrogenic common peroneal nerve injury while osteotomy and attempting to medialize the fibula into tibia in patients with extensive soft tissue fibrosis [4], [14]. In our case, the fibula had been osteotomized and lengthened before being medialized to the tibia. So, we did not encounter any difficulty during the medializing fibula and fixation fibula to the tibia. The common peroneal nerve was identified during fibular osteotomy. We did not encounter nerve injury complications in our case.
4. Conclusion
Leg lengthening then centralization of ipsilateral fibular graft is an excellent option for reconstruction of a tibial pseudarthrosis with a large leg-length discrepancy. It is a safe, rapid, inexpensive procedure. Our procedure was not difficult, microvascular skills and special devices were not required.
Funding
No financial support was received for the completion of this study.
Ethical approval
All procedures were approved by the 108 Central Military Hospital’s Institutional Review Board, Hanoi, Viet Nam.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Authors’ contributions
Dr. Doan Van Le: Conceptualization, Surgery, Writing – Review & Editing, Supervision.
Dr. Luong Van Nguyen: Conceptualization, Surgery, Writing – Review & Editing, Supervision.
Registration of research studies
Not applicable.
Guarantor
Dr. Luong Van Nguyen.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
The authors declare that they have no conflicts of interest.
Acknowledgments
The authors would like to acknowledge with gratitude the precious help of colleagues and the health staff of the Institute of Trauma and Orthopaedics at the 108 Central Military Hospital for the time required to prepare and implement this study.
Availability of data and materials
The data used to support the findings of this study are available from the corresponding author upon request.

